Nose Surgery (Rhinoplasty)
Consultations offered at our three convenient locations in Encino, Glendale and Bakersfield
One of the oldest plastic surgeries still in wide use today, the art of rhinoplasty has come a long way in the past few decades. Although it was once used to create a specific type of nose, today the primary focus of rhinoplasty is to create a nose that looks great and blends harmoniously with your existing facial features. Nose surgery can also be performed for reconstructive or functional purposes, restoring the nasal passages to ensure proper airflow.
Rhinoplasty is a delicate procedure that must be tailored to the needs of each individual. There are a wide variety of techniques that can be used to alter the shape of the nose. Dr. Younai helps each patient select the changes that will help them reach their goals, while ensuring that the nose will blend seamlessly with existing facial features. He firmly believes that the most attractive nose is one that allows the surrounding features to shine, without drawing particular attention to itself.
Contents
The Procedure
Rhinoplasty means “nose molding” or “nose forming.” According to the American Society of Plastic Surgeons, nearly 300,000 men and women underwent Rhinoplasty Beverly Hills in 2005 to improve the size and shape of their nose.
In addition to correcting breathing problems or injury. Rhinoplasty Beverly Hills can reduce or increase the size of your nose, change the shape of the tip of the bridge, narrow the span between its nostrils and alter its angle.
Rhinoplasty is more than surgery — it’s an art form. The plastic surgeon should create a nose that is yours uniquely and is harmonious with your face. Plastic surgeons generally recommend that patients wait until they are at least 14 or 15 to undergo Rhinoplasty.
The size and shape of your nose is largely inherited, and you may be unhappy with it for a number of reasons. Perhaps you don’t like its shape. Perhaps it’s out of proportion with your other facial features. Some people dislike the shape or position of their nostrils. Maybe the tip is too wide, pinched, large or bulbous. In the hands of a skilled plastic surgeon, these and other concerns can be addressed by “Cosmetic Rhinoplasty.”
The true function of your nose is to allow air to enter and exit the body. When nasal passageways are obstructed, breathing becomes difficult. A common cause of breathing problems is a deviated septum, a defect in the dividing wall in the nose. Some of the ailments associated with nasal obstruction are snoring, dry mouth, postnasal drip and nosebleeds. These can be relieved by “Corrective” Rhinoplasty, which includes Septoplasty to correct defects of the septum and widen nasal passages, and Turbinectomy to cauterize and trim the turbinates – the shelf-like lining of the nose, to create a balanced airflow. Also, Nasal Injury Repair Surgery corrects injuries to nasal bones and the nasal septum when they are fractured or disrupted. The timing of this surgery is crucial, as nasal bone fractures tend to heal quickly.
At one time, a “one nose fits all” approach to Rhinoplasty was the norm – with many patients having their noses “Westernized” to fit an outdated ideal of attractiveness. Today, Ethnic Rhinoplasty addresses the particular concerns of patients of varying racial and ethnic backgrounds, who wish to enhance their appearance while maintaining their ethnic identity.
According to the American Society of Plastic Surgeons, more than 1.3 million cosmetic surgeries were performed on ethnic patients in 2004, an increase of 44 percent since 2000. Among African American, Hispanic and Asian Americans, Rhinoplasty was one of the most commonly requested procedures. “Ethnic” traits addressed by Rhinoplasty include the dorsal hump and drooping tip often found on patients of Mediterranean descent (Jewish, Persian, Greek, Italian), the lack of cartilage in African American patients, the low or flat bridge in Asian patients and the weak broad drooping tip of many Hispanic patients.
A decision that you and you plastic surgeon will discuss is whether Open or Closed Rhinoplasty is best for you. During “open” or “external” Rhinoplasty, a small incision is made in the columella — the central column that separates the nostrils – and the nasal skin is lifted off the tip of the nose through this incision. During the more traditional “closed” Rhinoplasty, several cuts are made in the nostrils, and extending over the columella. One advantage of the “open” technique is that it allows the surgeon better exposure to the nasal anatomy. One advantage of “closed” Rhinoplasty is that it causes less disruption of the nasal tip blood supply, which lessens post-surgical nasal tip swelling, as well as reducing the risk of nasal tip complications.
Dr. Younai may utilize any number of techniques during your rhinoplasty procedure based on your individual needs. However, the basic steps of any nose surgery remain essentially unchanged. After deciding on the best course of action for you based on your consultation, your surgery will be scheduled.
Basic Steps
- The patient is usually put under general anesthesia.
- Incisions are made either inside the nostrils or on the outside of the nose. The placement of the incisions will depend upon the nature of your individual procedure and the anatomy of your nose.
- The soft tissues of the nose are raised up, allowing Dr. Younai to access the underlying structure.
- The septum might be adjusted, especially in cases of airway restriction.
- The soft tissues are draped back down and the nose is sutured.
The surgery is usually performed on an outpatient basis, so you should make arrangements to have someone drive you home that day. Rhinoplasty can help correct a number of issues, so your procedure will be unique to your individual needs.
Types of Rhinoplasty
Dr. Younai can perform a number of specialized nose surgery techniques to help you achieve your goals. No matter what your goals are there is a nose reshaping technique that can help you get facial harmony without losing your unique beauty. Some of the most common techniques include:
Septoplasty
This approach is used to correct a deviated septum. A deviated septum can make breathing through the nose more difficult and can be the result of injury. Common side effects of a deviated septum include snoring, postnasal drip, nose bleeds, and dry mouth.
Turbinectomy
This treatment is used to cauterize and trim the lining of the nose, also known as the turbinates. Like septoplasty, it is also commonly used to relieve a nasal obstruction.
Ethnic Rhinoplasty
Because most patients interested in cosmetic nose surgery have traditionally been of European descent, rhinoplasty was not suited for certain ethnicities in the past. People of African and East Asian descent have been particularly difficult to operate on in the past. However, a specialized branch of nose jobs known as Ethnic Rhinoplasty have developed new ways to give these patients the same options as other ethnicities.
Open Rhinoplasty
This designation has to do with the placement of the incision during surgery. In an open rhinoplasty procedure, the incision is made on the columella. This is the thin piece of skin that separates the nostrils. It allows the surgeon more visibility and access to the underlying tissues.
Closed Rhinoplasty
A closed rhinoplasty is performed by making the incisions inside the nostrils. This keeps them completely concealed from view. However, this incision type is not appropriate for all procedures.
Revision Rhinoplasty
When a nose surgery patient is unhappy with the results of their surgery, they may seek out a revision rhinoplasty operation to correct the previous procedure. Patients typically seek revision because the original nose job looks unnatural, usually as a result of an over-aggressive surgeon.
Revision Rhinoplasty is a “do over” of a nose upon which the original Rhinoplasty was unskillfully performed. In most cases, Revision Rhinoplasty is necessary because the original surgery was performed too aggressively, resulting in an “over operated” look.
You should be highly selective in choosing a plastic surgeon for Rhinoplasty, as it is one of the most surgically and aesthetically challenging procedures performed today.
While physicians such as Ear-Nose-Throat specialists (otolaryngologist) might be qualified to perform nasal surgery, they may lack the rich and broad-based knowledge and experience of a board-certified plastic surgeon, who is trained in all aspects of facial esthetic surgery.
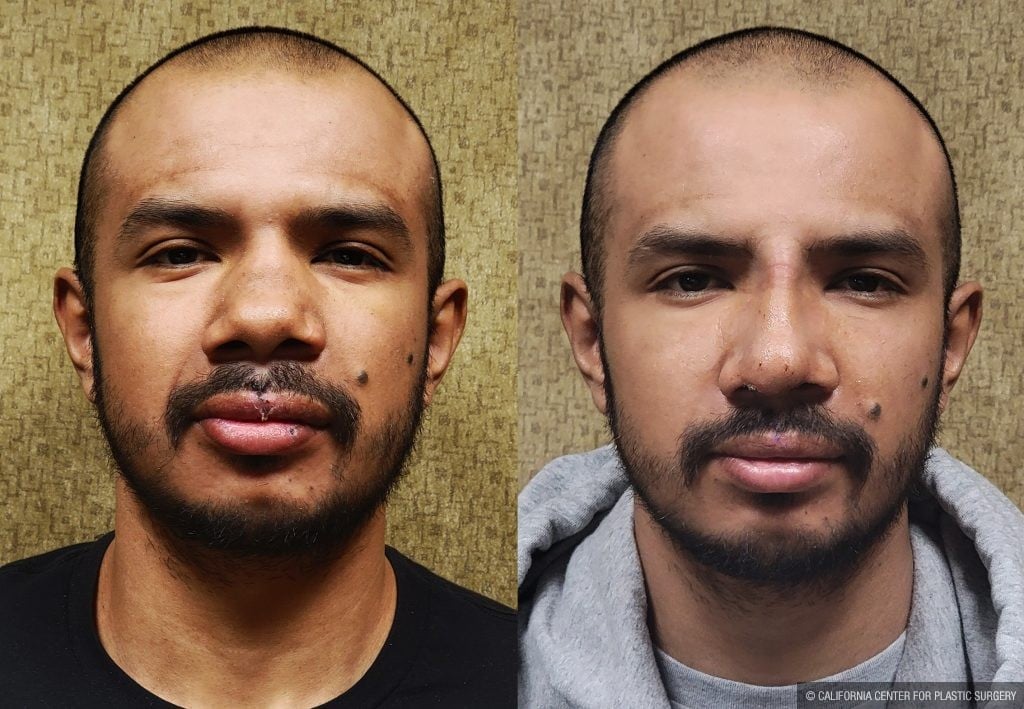
Before and After Photos
Surgical Techniques
Each rhinoplasty procedure is customized to the needs of the patient. There are many parts of the nasal anatomy, not all of which need to addressed in every patient. In addition, some patients need certain areas built up while others would benefit from reducing the size of these same features. And even the exact same nose can look drastically different on different faces.
In cases where the size of the tip or bridge needs to be augmented to achieve the desired look, Dr. Younai can use cartilage grafts taken from your ribs or ears. Nasal implants made from synthetic materials may also be an option. Otherwise, tissue is removed through incisions either below the columella (the piece of skin that separates the nostrils) or within the nostrils. These procedures are referred to as open and closed rhinoplasty, respectively. The proper technique for your rhinoplasty will depend on the adjustments being made. In either case, your scars should be small and nearly imperceptible.
Nose surgery to repair functional issues is slightly different. Blockages within the nasal passage are usually moved or removed, as in septoplasty or turbinectomy. If the internal nasal valve has deteriorated, spreader grafts made from your own cartilage can be placed on either side of the septum to allow optimal airflow.
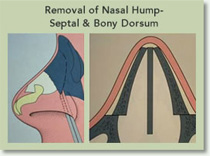
Remove the “Hump”
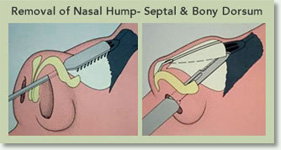
This is the most common type of Rhinoplasty. Made of bone and cartilage, the “hump” is whittled down by the plastic surgeon in order to make the nasal bridge straight and smooth. The decision of how far down to carve the hump depends on the patient’s other features, sex, and their preferences. Some patients prefer a more straight nasal bridge while others would like a softer look or a more “ski-sloped” nasal bridge.
Decrease the Tip
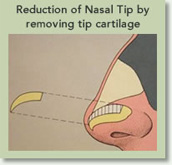
Decreasing a wide nasal tip is one of the most common changes made through Rhinoplasty. To achieve this, the plastic surgeon modifies the tip cartilages. The width or the length of the cartilage will be removed, depending upon the patient’s features. At time the nasal tip support is re-enforced with a cartilage “strut graft.”
Narrow Nasal Bones
The upper portion of your nose that is closer to your eyes is made of bone. Sometimes, the nose appears too wide. Many patients undergo Rhinoplasty to narrow that portion of the nose by fracturing the nasal bone at its base and moving them closer to each other. This is the part of the Rhinoplasty that generally people call “breaking the nose.”
Lengthen A Short Nose
The nose can be lengthened with the use of cartilage grafts that help restore the height and length of the nose. This procedure is mostly performed as an open approach.
Shorten a Long Nose

A long nose otherwise referred to as a “Pinocchio nose” appears long due to the over-projection of the nasal tip. This projection can be lessened and made more natural looking by mostly refining the tip structures of the nose, generally through an Open Rhinoplasty.
Candidates
Your nose — it’s the focal point of your face and a feature that defines your entire facial character. Rhinoplasty improves the size, shape, and the overall appearance of the nose so that it becomes more harmonious with your face. Transformation of your nose to one that is just right for you requires the utmost, skill, precision, and an instinctive sense of facial balance and uniqueness.
The term Rhinoplasty actually means “nose molding” or “nose forming.” According to the American Society of Plastic Surgeons, nearly 300,000 men and women had their noses reshaped in 2005. In addition to correcting nasal breathing problems, obstructions, or injuries, Rhinoplasty can also reduce or increase the overall size of your nose, change the shape and size of the tip or the bridge, change the size and shape of your nostrils, and alter its angle.
“Now I finally feel confident and no longer feel like I have to hide my profile!” — Lucy, age 32
From the time of the first documented “nose job” in 1597, surgery of the nose, or Rhinoplasty, has evolved from a procedure first developed to replace noses that were once amputated as a punishment for crimes, as well as those deformed and scarred by the ravages of socially ostracizing diseases, such as syphilis. The trends in Rhinoplasty have also evolved over the past decade. It is no longer performed to mask the ethnicity of men and women who sought acceptance through assimilation in their land of choice, but to actually refine and enhance their ethnic features.

Today, Rhinoplasty is an art form as much as it is a surgical procedure. A skilled cosmetic plastic surgeon will ask you: Which is the right nose for your face, and your face alone? Your surgeon must have an artistic sense. With this unique facial feature, it should never be “one size fits all.”
What troubles you about your nose? The sculpting of your nose requires thorough consideration of many factors. These include keeping your nose in harmony with all other facial features, while also considering your existing nasal structure, function, and physiology. Is there airway obstruction that needs correction? Has your nose suffered from injuries such as a fracture that needs correction? Do you get headaches or sinus troubles from chronic nasal airway obstruction? Will we be sculpting your nose for purely cosmetic reasons, or to restore its structure and function, or both? There are also men and women who undergo “Revision” Rhinoplasty – to correct previous nose surgeries that had poor outcome.
Good Candidates
While Rhinoplasty can enhance your appearance, it might not necessarily change your look to match your specific ideal, or cause others to perceive and treat you differently. Therefore, your decision to undergo Rhinoplasty has to be made very carefully, giving thorough considerations to what you want, and what is realistically possible. The best candidates for Rhinoplasty are those who are emotionally and psychologically mature, and are looking for improvements – not perfection.
Candidate Checklist
- Your nose might be too large for your face.
- Your nose might be too small for your face.
- You have a bump on the nasal bridge that shows on the profile view.
- You have a flat or shallow bridge (your glasses slip off your nose).
- You have a nose that seems too wide from the front view.
- You have a nasal tip that droops, plunges, or hangs excessively.
- You have a nasal tip that protrudes, like a “Pinocchio nose.”
- You have a nasal tip is too thick, large, bulbous, or boxy.
- You have a nasal tip that is too pinched or sharp.
- You have a nose that is crooked or off-center.
- You have flared or large nostrils.
- You have pinched or collapsed nostrils.
- You have problems breathing through your nose due to structural abnormalities and injuries.
- You have developed structural or functional nasal complications from previous surgeries.
Preparation
- Approximately one to two weeks before your surgery you will undergo a general pre-operative evaluation at our office, at which time you will also undergo blood testing and EKG if necessary.
- At that time you need to review with our staff all your medical conditions even though they might not appear to be of importance to you. The review of your eye and vision health is also crucial. We would like to know if you had previously undergone any nasal surgery, do you take any nasal sprays or allergy medications, and if you suffer from nasal airway obstruction, snoring, or apnea.
- After reviewing the procedure and answering your questions we will give you written instructions of the medications, vitamins, or herbs to avoid for at least two weeks prior and after your surgery. These include over the counter medications or vitamins which might thin your blood and cause you to bleed excessively during and after surgery.
- If you smoke we encourage you to reduce your smoking for one week before and after surgery because this can hamper your healing process.
- You will be provided with prescriptions for pain medications, antibiotics, and nausea medications. Please have these ready in advance.
- Get your house in order so that after surgery you wouldn’t be bothered with doing demanding house chores.
- Have bags of frozen peas or cold compresses ready in your freezer for use after surgery.
- Have your bed area prepared with many pillows or cushions to be used for propping you up. Elevation of the head after surgery reduces swelling and pain.
- Arrange for adequate support for the care of your children and pets for at least the first two to three days after surgery.
- You would not be able to wear heavy glasses that put pressure over your nose.
- Have someone reliable, preferably a family member or close friend bring you to surgery and from surgery. This person should be available to stay and assist you the night after surgery. If you don’t have such a person, please let us know in advance so that we can recommend several available after-care facilities or caretakers to you.
- Have loose and comfortable clothes and shoes available to wear the day of surgery. Especially, bring front open shirts so that you don’t have to pull them over your head when getting dressed after surgery.
- You cannot drink or eat anything except your medications for eight hours prior to surgery.
- Don’t drink any alcohol for one week prior and after your surgery.
- Do not wear any makeup, facial lotions, or perfume the day of surgery. Shower and shampoo the morning of surgery, remove all eyelid and eyebrow cosmetics, and don’t apply any hair gel or grease.
- Bring all your medications with you to surgery.
- Don’t wear jewelry, necklaces, tongue rings, body piercing, wristwatches, hairpieces, false eyelashes, or contact lenses to surgery.
- If you are to undergo septoplasty, turbinectomy, or sinus surgery, please have your post-op nasal rinsing setup prepared in advance. The setup instructions are provided in the post-op instruction section.
Recovery
Nasal Surgery is performed either under deep sedation or light general anesthesia. Most people don’t remember their experience in the operating room because of the amnesia effects of the sedatives.
After your surgery, you will spend some time in the Recovery Room of the surgical facility.
When you wake up, you will have a cold compress gauze dressing over your nose and eyes and a nasal splint on our nose. Don’t be alarmed if your eyes are covered and you cannot see. There is always a nurse available to assist you. Just ask for anything you need!
Your vision might also be blurry for few hours after surgery because of the lubricants that were placed on your eyes to keep them from drying during surgery.
Don’t panic even if you cannot breathe through your nose. You might either have a nasal packing or have swelling blocked your nasal airway. You will be able to continue to breathe through your nose, just like when you have nasal congestion with the flu.
After you go home you will experience some bloody discharge from your nose for several days. This is normal, unless you are bleeding profusely. Don’t pack your nose, stuff tissue paper in your nose, or stick Q-tips or fingers into your nose. You can cause more injury and bleeding.
You will have much bruising around your eyes which will gradually dissipate over the next two weeks.
It is normal to feel dizzy and to get nauseated during the first week of surgery, especially while you are taking narcotics. You can take your nausea medications, and make sure that you take your medications with food.
If you have nasal packing, please carefully follow the instruction for its care and removal provided in the following section.
Recovery Instructions
- After surgery, the best position for the first two days is to be lying semi-reclined. Elevation of the upper body and head reduces the swelling and aching of the nose.
- The application of cold packs or frozen peas over your eyes and nose are of the most benefit, especially during the first two to three days.
- Refrain from staying in hot places or in front of the oven or a heater because it can dry your nose and increase the chance of getting a nosebleed. In addition, you can help prevent excessive nasal dryness by using a humidifier, and applying Vaseline to your nostrils before going to bed and after getting out of the shower. Saline nasal sprays do help moisturize the nose, but because they dry quickly, they are not as effective as applying Vaseline.
- Take your pain medications routinely because any increase in pain can increase your blood pressure and cause nasal bleeding, more swelling, bruising, and prolonged healing.
- Take your nausea medications about one hour before taking your antibiotics and pain medication in order to lessen the extent of nausea.
- There are not dietary restrictions. However, you should refrain from eating greasy or acidic foods to prevent nausea. Make sure to drink adequate fluids so you do not get dehydrated.
- If you take high blood pressure medication, be sure to continue taking it to reduce the chance of a nosebleed.
- Do NOT take any aspirin-like products, diet pills, or vitamins until after approved by your doctor.
- It is good to stay well hydrated but avoid drinking too much plain water because it can make you more nauseated.
- Avoid eating greasy or spicy foods for the first three days, and have antacids available if you get an upset stomach.
- Refrain from smoking for at least two weeks after surgery, because smoking can actually irritate the eyes and prolong your recovery.
- Do NOT blow your nose forcefully, because this causes nosebleeds. If you are about to sneeze, keep your mouth open, to relieve nasal pressure.
- Don’t pack your nose, stuff tissue paper in your nose, or stick Q-tips or fingers into your nose. You can cause more injury and bleeding.
- You should keep your nasal splint dry and intact until removed by your doctor.
- I encourage you to be mobile and not to be sedentary in order to reduce the chance of forming blood clots in your legs.
- Recovery varies for each patient, as will the timing for resuming exercise and normal physical activities. Although you will probably be able to return to work within a 3-7 days, your cosmetic surgeon will instruct you to avoid heavy physical exertion, including heavy lifting, frequent bending, reaching high over shoulder, and jogging for the first 3-4 weeks.
- While most of the swelling will go away during the first two months, there is going to be some residual swelling and inflammation for up to one year after surgery depending on the extent of surgery and the way your body heals.
- You can have sex after one week, as long as you don’t overly exert yourself.
- You cannot use a public pool, Jacuzzi, or go into the ocean for at least 4 weeks after surgery.
- Small whitehead-like cysts called Milia can develop on your nose after surgery, which will go away by skin cleansing.
- Internal nasal sutures are dissolvable and do not have to be removed. If you have external sutures, they will usually be removed in about one week after surgery.
- You can wear camouflage makeup and concealer after your sutures are removed.
- After returning to work, do no drive or operate machinery if you are taking narcotics.
- If you get a nosebleed don’t panic and follow the instructions provided below.
- During your first week after your surgery if you have any urgent questions or concerns, please feel free to contact my office, at any time of the day or night.
Removing Nasal Packing
Patients who undergo nasal reconstruction, septoplasty, turbinectomy, or sinus surgery usually have their nose packed at the end of surgery with a special soft sponge that has a string attached to its end. In some ways it is like a feminine tampon. This packing will sooth the raw areas inside the nose, keep it from over-drying, and prevent scarring and bleeding.
After surgery the nasal packing will stay moist or even drip with watery blood, which is normal.
On the second day after your surgery, you are to remove your nasal packing with the help of your family and friends as described below. Don’t be scared, you can do it!
- Take two pain pills about one hour before removing your nasal packing.
- Wet your face and neck with water and stay somewhere cool and next to a sink.
- Wet your nasal packing, firmly hold on to the string of the nasal packing, and pull it out gradually and from side to side. This packing is usually the length of the finger. It is best to pull it out slowly but firmly and continuously. Keep your mouth open when doing this.
- After the nasal packing is removed, it is not unusual to get a little nosebleed. If so pinch the soft part of your nose for 5 minutes, while keeping your head elevated. The bleeding almost always stops.
- Later on, and usually four times a day for two weeks you need to irrigate your nose with tap water. This will help wash away the blood clots from inside of the nose and to keep nasal discharge and blood to get hard and stuck to the inside of your nose.
- The best tool for irrigation is to use a soft bulb irrigator which is usually used to clean the baby’s nose. Fill it up with tap water, place the tip of it at your nostril, aim it towards the back of your neck and flush forcefully while your mouth is open and your head is over the sink. The water would usually come out from the other nostril as well as your mouth. Repeat this several times a day.
- After irrigation, in order to keep your nose from drying, apply some Vaseline at your nostril and sniff. This will coat the inside lining of the nose and will keep it from drying. Repeat this after your leave the shower.
- After you remove your nasal packing, and irrigate your nose, DO NOT blow your nose forcefully, because this will cause a nosebleed.
Nosebleeds

- DON’T panic! Excessive excitement will raise your blood pressure and worsen the bleeding.
- Pinch the soft part of your nose between your thumb and index fingers for about 5 minutes.
- Take two pain pills (No aspirin or anti-inflammatory pills).
- Wash your face and neck with cool water. Stay in a cooler place and don’t drink anything warm.
- Don’t lie down or put your head down. In fact, keep your head elevated so that blood doesn’t rush to your head.
- Refrain from coughing, sneezing, retching, or blowing your nose.
- If nasal bleeding continues, or keep re-occurring, call your doctor immediately.
Tips for Your Significant Others
The support of your family and loved ones can be as important to your healing as following your physician’s medical directives. Their understanding of the pain, discomfort, and at times, the roller coaster of emotions, that you might experience can make all the difference in having an optimal outcome.
Here are some tips for your significant others that will be helpful to them in helping you:
- You should be available as a full time caregiver for at least 24 hours to help the patients with the tasks that are normally taken for granted, like being able to walk to the bathroom.
- You, or someone, should care for the patient’s children for a minimum of two days, and be sure that she has assistance in lifting young children for several days after your surgery.
- Help with pet care. Someone should walk them, feed them and clean up after them for at least several days.
- Read the Postoperative instructions above. It will be helpful to the patient for you to assist him or her in the removal of the nasal packing about one and one half days following surgery, and to assist the patient with the nose irrigation described. They may also need your assistance should a nosebleed occur, and with reminders to sleep with their head elevated for the first 2-4 days.
- Know that the patient may experience mood swings, and feel like crying off and on – especially in the first couple of weeks. This is a normal aftermath of major surgery.
- Encourage the patient to stay hydrated by drinking lots of water.
- Remind him/ her to not fight the pain – he/ she should go with the flow, and take his/ her medications as directed. It is not good to try and be a hero!
- Give the patient lots of compliments. A patient is sometimes fearful because it will take some time before the nose appears as it will with time. There is a lot of healing to do!
- Prepare simple and easily digestible foods, such as scrambled eggs or Jello.
Revision
There is variety of reasons to seek Revision Rhinoplasty. Some patients are looking for further enhancement and refinement of their nose after their first surgery. Others are not happy with the change in their look, or expected to get a different nose with their first surgery. They might feel that their new nose does not fit the rest of their face or changes their look drastically.
There are times when the initial surgery distorted some of the nasal structures, as well as having adversely affected nasal function. For example, the nasal bridge collapsed ( Saddle Nose Deformity) or the nostrils became over-pinched (“Pinched Nose Deformity”), the nose became crooked, or even the nose became obstructed. Some of these events were caused by the initial surgical technique, while others arose out of the inherent characteristics of the nasal cartilage and soft tissue. For instance, it is known fact that nasal cartilage can warp by itself, thus making the nose crooked.
Revision Rhinoplasty usually involves a number of highly specialized techniques, and possibility reconstruction with multiple grafts, harvested from the septum, ear cartilage, or even the rib cage.
“A few years ago, I had a Rhinoplasty performed overseas to get rid of a hump that I had on the left side of my nose. When I came home, I saw that my nose was crooked whereas it had been straight before, and one side looked as if it had collapsed. It was totally uneven and disfigured. I cried every night for months and kept hoping it was a bad dream. Now, I am so happy with the results of my Revision Rhinoplasty. Everything that needed to be fixed was fixed, and it turned out great.” — Judy, age 36
The decision to undergo Revision Rhinoplasty should be taken very carefully, and after extensive discussion of expectations, existing nasal anatomy, limitations, and treatment options.
Nasal Implants
Rhinoplasty or nose surgery performed on most Caucasian usually involves some sort of reduction in the size of the nose. In particular, the nasal hump, or the large nasal tip is reduced.
On the contrary, rhinoplasty for most Asians and African-Americans involves enlargement or augmentation of the nose! In these cases the flat nasal bridge is heightened or the projection of the nasal tip is increased. This requires a different type of rhinoplasty, one that involves use of nasal implants.
Candidates
Nasal implants are generally used to augment the nasal dorsum or bridge. Many Asians and those of African descent don’t have prominent noses and at times are deficient in the height of the nasal bridge. In addition to wanting to enhance and balance their facial features, they often complain that their glasses slip off their nose because they don’t have a strong nasal bridge!
Esthetically speaking, lack of nasal dorsal or bridge height tends to make the nose look short and fat. It also makes the eyes appear too far apart. Finally, lack of forward nose projection also tends to make the face look too flat and round. Augmentation of the nasal bridge will help elongate the nose and gives the face a more refined and balanced appearance.
Materials
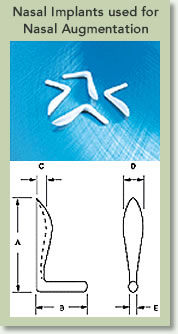
Most plastic surgeons prefer to used natural material for nasal augmentation, especially that from the patient themselves. This material is called an autologous graft, and is often harvested from the nasal septal cartilage, ear cartilage, ribs, or bone. While autologous grafts have the advantage of better acceptance by the patient’s body and less chance of infection; they do partially re-absorb or shrink. Besides requiring added surgery to harvest these grafts from a patient’s body, often the amount of tissue available for harvest might be limited and not enough to achieve the desired augmentation. On the other hand, synthetic grafts or implants are abundant and come in a variety of shapes and sizes. They don’t require added surgery to harvest a graft, and don’t re-absorb or shrink after implantation. Unlike autologous grafts, synthetic nasal implants carry a higher chance of infection or extrusion. These implants are typically made from Silicone, Gortex or PTFE.
Ethnicity
For many years, a “one size fits all” approach was taken to nose reshaping, and this also applied to the type of implants that were used. “Caucasian” implants were used on all patients.
Today, however, cosmetic surgeons tailor implants according to specific facial characteristics of various ethnic groups, including African-Americans, Hispanic, and Asian patients. For example, an implant used for an Asian is usually slimmer and smaller than one used for a typical African-American.
A skilled cosmetic surgeon will choose the appropriate implant size and shape, and might even carve and modify them to customize it for the patient’s ethnic traits and specific facial features.
Nose Augmentation with Nasal Implants
This is a procedure that should be performed only by a highly skilled plastic surgeon, with experience in ethnic nasal surgery or rhinoplasty. Generally, the surgery involves the creation of a nasal pocket for insertion of the specially designed implant. The incision is made inside the nose, with dissection along the dorsum or top of the nose to create the appropriate space for the implant. Rarely, sutures are used to hold these implants in place; instead a tight fit pocket will hold in the nasal implant in the appropriate place. After surgery, the implant is kept in the correct place by wearing a nasal splint for a week.
Adjunct Procedures for Nasal Augmentation
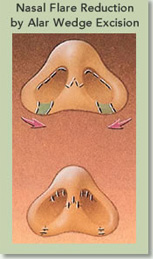
Besides augmenting the nasal dorsum, often times, the flare of the nasal ala or the nostrils are reduced. This is accomplished by making an incision in the nasal alar crease, removing excess ala, and reducing the size of the nostril opening.
Sometimes nasal “strut grafts” are used as a “post” to increase the height and projection of the nasal tip. Other times, grafts are used in the pre-maxilla, or the area between the nose and the upper lip, in order to reduce the appearance of a sunken mid-face.
Anesthesia
Nasal augmentation is an outpatient surgery that can be performed under sedation or with general anesthesia. The procedure takes about one hour, and usually the patient can be back at their usual activities within one to two days.
Risks
In general nasal augmentation is a very safe procedure. Typically, the nasal implant surgeries that carry a higher risk for complications are revision surgeries. It is not unusual to encounter people in such circumstance who have had a history of multiple nasal surgeries. In these instances the circulation to the nasal skin is sub-optimal, thus there is a higher chance for implant extrusion or displacement, infection, skin breakdown, and scarring. The best way of minimizing complications with nasal implant surgery is to have realistic expectations, use autologous grafts when feasible, and to seek a plastic surgeon who has had adequate experience in nasal implant surgery.
Ethnic Rhinoplasty
According to the American Society of Plastic Surgeons, more than 1.3 million cosmetic surgeries were performed on ethnic patients in 2004, an increase of 44 percent since 2000. Among African American, Hispanic and Asian American patients, Rhinoplasty was one of the most commonly requested procedures.
“As Jews became more and more unwelcome in Germany before WWII, Dr. Joseph offered to perform a free Rhinoplasty for any of his fellow Jews who didn’t want to stand out in German society.” — Article in the Jewish Review, 2004
In the majority of cases, and unlike times past when aesthetic surgery was tailored to Caucasian faces, the majority of these patients wish to enhance their appearance while maintaining their ethnic identity. As fashion changed, and ethnic models began gracing the cover of magazines in the 1970’s, blondes weren’t the only ones having fun anymore! Patients began seeking enhancement, while maintaining their unique racial and ethnic profile.
In short, no longer do skilled plastic surgeons do the same operation for all ethnicities. Rather, an experienced and skilled plastic surgeon will be aware of how ideals of beauty differ between various ethnic groups. Whereas fifteen years ago, a Rhinoplasty was “one size fits all,” with surgeons giving a similar nose to all of their patients, today we thrive to maintain facial harmony while enhancing the ethnic nose.
While each patient is unique, there are specific features characteristic of “ethnic” noses.
Mediterranean Patients
These include patients of Persian, Arab, Jewish, Italian or Greek heritage. Many of them have a dorsal hump (the dorsum is the region between the tip and the forehead) and a drooping nose tip. In these cases, the plastic surgeon will elevate and narrow the tip, while lowering and narrowing the dorsum.
African American Patients

African American patients often have little or no cartilage in the tip of the nose, lack of nasal bridge projection, flared and large nostrils.
African American Rhinoplasty is very different than that performed on other ethnic groups. It focuses on building up the bridge of the nose and also on the reduction of the nostrils. Rather than removing cartilage or bone, the plastic surgeon builds up the nose tissue. This might be done through nasal implants, made of silicone or Gortex, or through grafts made of cartilage from the patient’s septum or ear. Surgery elevates the dorsum, and narrows and projects the tip. Sometimes, the plastic surgeon uses cartilage from the septum or the ear to build up the dorsum or project the tip.
Asian Patients
Unlike Caucasians who usually require reduction, Asians generally require augmentation of the nose. Many Asian patients have a low or flat bridge, which needs to be built up. Often, tissues are taken from the patient’s septum, and used to build up the dorsum, or modify and enhance the tip. Where no tissue is available from the septum, the surgeon may take tissue from the ear or the scalp. Sometimes, the surgeon will use a nasal implant.
Hispanic Patients
Many Hispanic patients have a weak broad drooping tip that hangs over the upper lip, a dorsal hump, and a retracted columella. The plastic surgeon will elevate and narrow the tip, while removing the bump.

Dr. Younai is a Board Certified Plastic & Reconstructive Surgeon with experience in all aspects of Facial Cosmetic Surgery including that of the Nose, Sinuses, Eyes, Ears, Chin, Cheek, etc. He is skilled and experienced in all techniques of Rhinoplasty and Sinus Surgery, and strives to create the nose that is natural looking and harmonious with the rest of your face. In doing so, he tries to preserve patient’s Ethnic Features while enhancing their overall facial appearance.
Asian Nose Surgery
Asian Rhinoplasty differs significantly from nose surgery of Caucasians in Los Angeles. In fact, it takes specialized training and expertise as a Board Certified Plastic Surgeon to truly master Asian nose surgery. The reason is that there are many fine differences between an Asian nose and that of other ethnicities. The following are some of characteristics of an Asian nose which make Asian nose rhinoplasty unique and challenging.
Nose Bridges
In general, most Asians from Korea, China, Philippines, Japan, Hawaii, and Malaysia have underdeveloped nasal bridge. This makes their eyes appear to be far apart. While in Caucasians nasal septal cartilage is used to augment nasal bridge, in Asians septal cartilage is often small and thus an inadequate source of autologous graft. Ear or Conchal cartilage is also not sufficient. In China or Korea rib cartilage is often used to augment nasal bridge with excellent aesthetic results, but this could leave a bad scar below the breasts, besides, removal of a rib is painful. Therefore, most plastic surgeons that specialize in Asian Rhinoplasty in Beverly Hills often use synthetic nasal implants made from silicone, Gortex, or Medpore.
Nasal Implants
Nasal implants that are used for the augmentation of the nasal bridge and tip in oriental or Asian rhinoplasty are often made from silicone, Gortex, or Medpore. Gortex usually comes in sheets which have to be carved and assembled. It usually gives a very soft and nice result, but it might be too soft of an implant to provide enough nasal tip projection. On the other hand, Medpore implants are often too hard and brittle. Medpore has a higher chance of extrusion. Silicone nasal implants are most popular due to the fact that they come in many different sizes and shapes. Silicone nasal implants can be further carves and shaped before insertion into the nose. All synthetic nasal implants have the potential risk of extrusion. This is usually uncommon with exception of instances when there was trauma to the nose, poor circulation, or when the implant was excessively manipulated from the outside.
Nasal Tip Shaping
The nasal tip in Asians is often round, wide, bulbous, and of poor definition. The thickness of Asian nasal skin also contributes to the lack of nasal tip sharpness. During Asian Rhinoplasty nasal tip can be refined by manipulating its existing cartilage, as well as by use of nasal dorsum and/or columella autografts or implants.
Narrowing of Nostrils
Nostrils in Asians can be flared and wide. During Asian Nose surgery the size and shape of the nostrils can be made smaller and narrower by an alar wedge resection. This technique of Asian Rhinoplasty has to be performed in a careful way neither to make the nostrils look too pinched, nor to make the nasal tip look like a triangle.
Lengthening of the Nose
ack of nasal bridge height can give the appearance of a short nose. During Oriental Rhinoplasty a combination of augmenting the nasal bridge and raising the nasal tip helps to make the nose look longer, slenderer, and balanced.
Complications
Every surgery including nose surgery on Asians carries certain risks and potential complications.
Q & A
Is there a minimum age to undergo Rhinoplasty?
The size and shape of a nose change during adolescence. Therefore, plastic surgeons generally recommend waiting until at least 15 years of age to consider Rhinoplasty. Boys should generally wait longer because they complete their developmental phase later than girls.
An exception to this rule is a baby that is born with congenital facial deformity such as a cleft lip. In this child, surgical corrections are made to the nose very early on so that the nose will grow in a normal fashion.
What Facial Features Can Affect the Appearance of the Nose?
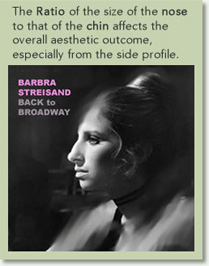
The proportion of a nose to that of the rest of the face, especially when viewed from the side, is closely linked to the proportions of the chin. Often times a weak chin can make a nose appear too large for the face, or vice versa.
Attention to this relationship is very important in the assessment of the nose and surgical planning. There are times that surgery on the chin (Genioplasty) is an essential adjunct to a Rhinoplasty. At this time, the chin can be augmented or brought forward (Advancement Genioplasty), or reduced or pushed backwards (Reduction Genioplasty or setback).
The size, angle, and flow of the upper lip can also affect the appearance of the nose. Those with a very deep space between their upper lip and the nose, often appear to have an excessively hanging or drooping nasal tip. Augmentation of this area can change the angle between the nose and the lip, and thus significantly alter the overall appearance of the nose. On the other hand, those with thin and long upper lips can appear to have a short nose. Correction of this can also affect the appearance of the nose.
The shape of the eyes, especially that of the inner corners of the eyes (medial canthus), can affect the appearance of the nasal bridge, and vice versa. For example, a flat nasal bridge can make the eyes appear to be too far apart, as is true for many Asian patients. The medial canthal folds in Asians can also make the nasal bridge to appear too wide and flat.
“Before my nose job, I always used to cover my nose, when I smiled or laughed. My nose tip used to hang down like a hook! After having had surgery, I now feel much more comfortable with my looks, and definitely more confident.” — Linda, age 25
The first intranasal Rhinoplasty was performed in the 19th century on a young man whose large nose caused him so much embarrassment, he was afraid to appear in public.
The size and shape of your nose is largely an inherited characteristic. Bone and cartilage create the skeletal foundation of your nose, over which skin is draped.
Rhinoplasty can reduce the skeletal structure of a large nose by removing the nasal hump or by narrowing the bony and cartilaginous structures. On the other hand, in those with lack of nasal projection or flat nasal bridge such as those of African or Asian descent, the nasal framework can be augmented with a graft or an implant. The nasal bony and cartilaginous frame structure can also be straightened in the case of a crooked nose while the shape and slope of the bridge can be made more natural.
Rhinoplasty can also alter the size, shape, projection, and the angle of the nasal tip. A hanging nasal tip can be lifted and the angle between the nose and the lip can be altered. A small pinched tip can be made more natural looking, while an overly projected “Pinocchio” tip can be reduced. A wide, boxy, or bulbous nasal tip can be shaped to a more natural form.
Rhinoplasty can also reduce the size of the large and flared nasal nostril, or open and widen a pinched nostril.
Cosmetic Rhinoplasty is performed by either an “open” or “closed” technique. With the “open” technique, the plastic surgeon reaches the nasal bones through incisions inside the nostrils and across the columella – the tissues separating the nostrils. With “closed” Rhinoplasty, the surgeon accesses nasal bones through an incision inside the nostrils, and then lifts the skin away from the underlying bones and cartilage. Some call this a “Scar-less Rhinoplasty.”
As a rule, surgery performed for purely cosmetic reasons will not be covered by your insurance. However, for many men and women these issues of appearance are very painful, even if they are not physically painful. For many, knowing that they can change their appearance is liberating. Many patients tell me that their only regret is that they didn’t have Rhinoplasty sooner!
“My breathing woke me up at night and got worse and worse. But I didn’t know anything could be done about it. I tried every new pillow, antihistamine and breathing strip I could find. I had developed the habit of breathing through my mouth. At last I had this surgery. Now I sleep like a baby.” — Ralph, age 50
We breathe, smell, and even taste with our nose!
The true function of your nose goes beyond just breathing, and its function is related to that of the sinuses, ear and the throat. When nasal passageways are obstructed, not only does breathing become difficult, but also the sinuses and the pressure balance of the ears are affected. That is why patients with chronic nasal airway obstruction also often suffer from chronic sinus and even ear infections.
Patients with nasal airway obstruction are often complaining of inability to breathe through one or both nostrils at night or during sports, post-nasal drip, dry mouth, sinus headaches, and pressure.
The obstruction of the nasal airway occurs at several levels. Constriction or collapse of the nostrils can present the initial level of nasal airway obstruction. Afflicted patients have learned to use splints or tapes to keep their nostrils open while sleeping. In fact, they often demonstrate improved breathing by just manually pulling away their nostrils. This deformity is often caused by the collapse or the constriction of the external nasal valve as a result of trauma or previous nasal surgery. It can be corrected in a variety of ways with the use of cartilage grafts such as a “spreader graft”, or a “batten graft.”
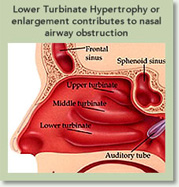
The next level of nasal airway obstruction occurs deeper and at the level of nasal septum and inferior turbinates. The nasal septum is a wall-like structure that divides the two nasal passageways. It is made of cartilage and bone that is covered in nasal mucosal lining. There are many people that are either born with a deviated nasal septum or develop it as a result of trauma or surgery. The combination of a deviated septum and enlarged inferior turbinates can severely obstruct the nasal airway. The septum can be straightened and the crooked parts removed in a procedure called Septoplasty. It is not uncommon to also harvest part of the nasal septum cartilage during a cosmetic Rhinoplasty to augment parts of the nasal skeleton.
The inferior turbinates are a pair of three levels of turbinates that help to humidify and regulate the flow of air. Either inherent enlargement and/or inflammation can result in significant enlargement of the inferior turbinates, thus blocking the nasal airway. This obstruction is alleviated by reducing the size of the inferior turbinates by a procedure call Turbinectomy. While some surgeons cut down part of the turbinates, others use electric cautery or radiofrequency energy to shrink them. Turbinectomy is a procedure that must be performed with the utmost care by a skilled surgeon who is highly experienced in the procedure, as the over removal of the turbinate can result in “Empty Nose Syndrome” (ENS). Symptoms of ENS include shortness of breath, chest tightness, breathing problems, abnormal heart rate, and the inability to control breathing. These symptoms are difficult to address as the turbinate tissue doesn’t regenerate.
In conjunction with these procedures the maxillary or frontal sinuses can also be assessed and cleaned through sinus endoscopy.
Nasal Injury Repair Surgery corrects injuries to nasal bones and the nasal septum when they are fractured or disrupted. The timing of this surgery is crucial as nasal bone fractures tend to heal quickly. As a rule, nasal Injury Repair Surgery is performed through a “closed” technique where skin incisions are not necessary. In those with very severe nasal skeletal collapse “open Rhinoplasty” will provide better access to the nasal skeleton.
“I was in a terrible car accident that broke my nose 15 years ago. Until I had this surgery, all I could see when I looked in the mirror was my misshapen nose. My self-esteem was horrible, and I stopped socializing. Now, I’m happy to look in the mirror, plus I can breathe clearly for the first time since the accident!” — Dana, age 31
Today, plastic surgeons can also restore “over-operated” areas by harvesting septal or ear cartilage and grafting it into a tiny pocket made inside the nose to correct certain deformities such as that of the bridge such as a “Saddle Nose Deformity“, or that of the tip via Tip Rhinoplasty.
Depending upon the patient’s needs, Tip Rhinoplasty can reduce or increase the size of the nasal tip, narrow the width of the nostrils, or change the angle between the nose and the upper lip. Tip Rhinoplasty can also help correct birth defects.
“Open” vs. “Closed” Rhinoplasty. Which one is better?
A decision that you and your plastic surgeon will have to discuss is whether the “open” or “closed” technique of Rhinoplasty is best for you — closed being the more traditional kind.
Closed Rhinoplasty
In Closed Rhinoplasty an “endo-nasal” incision is made in the nostrils. This incision is not visible and it provides a plastic surgeon great access to most of the structures of the nose for refinement. Closed Rhinoplasty is a more challenging and demanding technique for most plastic surgeons. Those that use this technique are usually more experienced and are skilled to manipulate the internal nasal structures through only an intra-nasal approach, without having to “open the nose.”
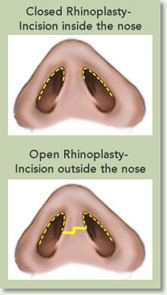
One of the major advantages of the Closed Rhinoplasty is that there are no external nasal scars, thus sometimes being called “Scar-Less Rhinoplasty.” Another advantage is that which this approach there is less swelling and faster recovery of the nose.
In my experience, most Rhinoplasties can be performed with this technique with the exception of some patients who need to have extensive work done on the framework of the nose and the tip.
Open Rhinoplasty
In “open” or “external” Rhinoplasty, a small incision is made in the columella, the central column that separates the nostrils. This is also known as a “trans-columellar” incision. The skin of the columella is very thin and the plastic surgeon makes a very short incision, which should be practically invisible following healing. It is through this incision that the nasal skin is lifted off the tip of the nose. It’s this one extra incision at the nose’s base that separates it from “closed” Rhinoplasty. Other incisions are hidden up inside the nose.
The advantage of this approach is that it gives the greatest visibility and access to the structures of the nasal tip. Therefore, in cases where there is need for extensive reshaping of the nasal tip, this might be a preferred approach.
The disadvantage of Open Rhinoplasty is the scar over the columella and the longer time that it takes for the swelling of the nasal tip to subside.
Is The Nose Packed After a Rhinoplasty?
A typical cosmetic Rhinoplasty does not require nasal packing and patients are able to breathe through their nose immediately. Despite this, there is going to be some drainage of blood and mucus from the nose that can obstruct the nose if not cleaned routinely.
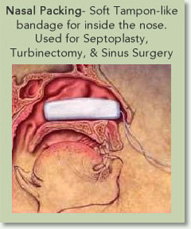
With a Functional Rhinoplasty that involves a Septoplasty and Turbinectomy, the nose is packed with a soft moist sponge which is similar to a tampon. This packing is basically the bandage for the surgery that is performed for the internal nasal structure. It prevents formation of scars and adhesions between different nasal structures, and lessens the chance of bleeding. I usually instruct my patients to remove this packing in one and a half days after surgery and to start cleaning and irrigating their nasal passageway then.
Risks & Complications
Rhinoplasty, Septoplasty, Turbinectomy & Repair Of Nasal Fracture
Surgeries of the nose- Rhinoplasty, Septoplasty, Turbinectomy, or repair of nasal fracture, are operations frequently performed by plastic surgeons. There is not a universal type of nose surgery that will meet the needs of every patient. These nose surgeries are customized for each patient, depending on his or her needs. Incisions may be made within the nose or concealed in inconspicuous locations of the nose in the Open Rhinoplasty procedure. In some situations, cartilage grafts, taken from within the nose or from other areas of the body may be recommended in order to help reshape the structure of the nose. Internal nasal surgery to improve nasal breathing can be performed at the time of the Rhinoplasty.
Nasal surgery like every surgical procedure involves a certain amount of risk and it is important that you understand these risks and the possible complications associated with them. In addition, every procedure has limitations. An individual’s choice to undergo a surgical procedure is based on the comparison of the risk to potential benefit. Although the majority of patients do not experience the following complications, you should discuss each of them with your plastic surgeon to make sure you understand the risks, potential complications, and consequences of Rhinoplasty.
Bleeding
It is possible, though unusual, to experience a bleeding episode during or after surgery. Post-operative nasal bleeding is probably the most common complication of rhinoplasty. Although in majority of cases this is very minor in some instances it may require emergency treatment to stop the bleeding, drain the accumulated blood, and/ or transfuse blood. Hypertension (high blood pressure) that is not under good medical control may cause bleeding during or after surgery.
Taking any aspirin or anti-inflammatory medications for ten days before or after surgery, as well as, non-prescription “herbs” and dietary supplements can increase the risk of surgical bleeding.
Heparin or Coumadin medications that are used to prevent blood clots in veins can produce bleeding. If blood transfusions are necessary to treat blood loss, there is the risk of blood-related infections such as hepatitis and HIV (AIDS). Accumulations of blood under the skin may delay healing and cause scarring.
Infection
Infection is very unusual after surgery. Should an infection occur, additional treatment including antibiotics, hospitalization, or additional surgery may be necessary.
Prolonged Swelling
It is normal for a nose to stay swollen from 8-18 months after surgery. This can be worse in cases of revision or open rhinoplasty. Patients need to be patient during phase of nasal healing. Use of steroid injections and topical medications to hasten this process can potentially result in more harm.
Scarring
All surgery leaves scars, some more visible than others. Although good wound healing after a surgical procedure is expected, abnormal scars may occur within the skin and deeper tissues. Scars may be unattractive and of different color than the surrounding skin tone. Scar appearance may also vary within the same scar. Scars may be asymmetrical. There is the possibility of visible marks in the skin from sutures. In some cases, scars may require surgical revision or treatment.
Change in Skin Sensation
It is common to experience diminished (or loss) of skin sensation in areas that have had surgery. There is the potential for permanent numbness within the nasal skin after rhinoplasty. The occurrence of this is not predictable. Diminished (or loss) of skin sensation in the nasal area may not totally resolve after rhinoplasty.
Asymmetry
The human face is normally asymmetrical. There can be a variation from one side to the other in the results obtained from rhinoplasty. Also, during the recovery phase, the two sides of the nose might swell, bruise, or scar to a differing degree, resulting in temporary or prolonged asymmetry. Nasal cartilage has a tendency to warp, therefore, there is a chance that warping of nasal cartilage graft or septum can result in asymmetry. Additional surgery may be necessary to attempt to revise asymmetry.
Skin Discoloration / Swelling
Some bruising and swelling normally occurs following rhinoplasty. The skin in or near the surgical site can appear either lighter or darker than surrounding skin. Although uncommon, swelling and skin discoloration may persist for long periods of time and, in rare situations, may be permanent.
Seroma
Fluid accumulations infrequently occur in between the skin and the underlying tissues. Should this problem occur, it may require additional procedures for drainage of fluid.
Pain
You will experience pain after your surgery. Pain of varying intensity and duration may occur and persist after rhinoplasty. Chronic pain may occur very infrequently from nerves becoming trapped in scar tissue.
Skin Sensitivity
Itching, tenderness, or exaggerated responses to hot or cold temperatures may occur after surgery. Usually this resolves during healing, but in rare situations it may be chronic.
Nasal Septal Perforation
Infrequently, a hole in the nasal septum will develop. The occurrence of this is rare. Additional surgical treatment may be necessary to repair the nasal septum. In some cases, it may be impossible to correct this complication.
Nasal Airway Alterations
Changes may occur after a rhinoplasty or Septoplasty operation that may interfere with normal passage of air through the nose. This could arise from recurrent septal deviation, recurrent turbinate hypertrophy, scar formation, or cases of internal or external nasal collapse. Although this does not occur frequently, it can be corrected by surgery.
Dry nose/ Empty Nose Syndrome
After undergoing nasal airway obstruction surgery, there might be a temporary or prolonged period of excessive dryness of the nose leading to nasal irritation, crusting, or even minor bleeding. This occurs as a result of alteration in the nasal airway flow. In most cases it is temporary, and can be managed by use of nasal irrigation and lubrication. In rare cases it might be permanent.
Distortion in External Nasal Appearance
Distortion in the projection of the nose may result from a Septoplasty. If this occurs, additional surgery would be necessary to correct this problem.
Residual Septal Distortion
It may not be possible to completely resolve distortions within the nasal septum with surgery.
Snoring Disorders
Snoring disorders may be caused by a variety of factors. Septoplasty may not relieve the propensity of some individuals to snore. Rhinoplasty does not affect snoring.
Skin Contour Irregularities
Contour irregularities may occur. Residual skin irregularities at the ends of the incisions or “dog ears” are always a possibility and may require additional surgery. This may improve with time, or it can be surgically corrected.
Sutures
Most surgical techniques use deep sutures. You may notice these sutures after your surgery. Sutures may spontaneously poke through the skin, become visible or produce irritation that requires removal.
Cartilage Grafts
Cartilage grafts may be needed if the goal of surgery is to change the projection of the nasal tip. These grafts can be obtained from donor locations within the nose (nasal septum), from other parts of the body, or from tissue banks. Complications including nasal septal perforation may occur from the procurement of cartilage graft material. More than one location may be needed in order to obtain sufficient amounts of cartilage.
Extrusion of Cartilage or implants
In cases when nasal implants, cartilage, or bone grafts are used, there is a risk that they might be rejected or expelled by your body. In this instance they can gradually extrude through your incisions or nasal skin. Smoking, trauma, substances that can hinder healing (i.e. steroids), and multiple nasal surgeries can increase the chance of such complication.
Delayed Healing
Fracture disruption or delayed wound healing is possible. Some areas of the nose may not heal normally and may take a long time to heal. Areas of skin may die. This may require frequent dressing changes or further surgery to remove the non-healed tissue. Smokers have a greater risk of skin loss and wound healing complications.
Damage to Deeper Structures
There is the potential for injury to deeper structures including nerves, tear ducts, blood vessels, and brain during any surgical procedure. The potential for this to occur varies according to the type of rhinoplasty procedure being performed. Injury to deeper structures may be temporary or permanent.
Allergic Reactions
In rare cases, local allergies to tape, suture materials and glues, blood products, topical preparations or injected agents have been reported. Serious systemic reactions including shock (anaphylaxis) may occur to drugs used during surgery and prescription medications. Allergic reactions may require additional treatment.
Surgical Anesthesia
Both local and general anesthesia involve risk. There is the possibility of complications, injury, and even death from all forms of surgical anesthesia or sedation.
Substance Abuse Disorders
Individuals with substance abuse problems that involve the inhalation of vasoconstrictive drugs such as cocaine are at risk for major complications including poor healing and nasal septal perforation.
Unsatisfactory Result
Although good results are expected, there is no guarantee or warranty expressed or implied, on the results that may be obtained. You may be disappointed with the results of rhinoplasty surgery. This would include risks such as asymmetry, loss of function, structural malposition, unacceptable visible or tactile deformities, unsatisfactory surgical scar location, poor healing, wound disruption, and loss of sensation. It may be necessary to perform additional surgery to attempt to improve your results.
Shock
In rare circumstances, your surgical procedure can cause severe trauma, particularly when multiple or extensive procedures are performed. Although serious complications are infrequent, infections or excessive fluid loss can lead to severe illness and even death. If surgical shock occurs, hospitalization and additional treatment would be necessary.
Cardiac and Pulmonary Complications
Surgery, especially longer procedures, may be associated with the formation of, or increase in, blood clots in the venous system. Pulmonary complications may occur secondarily to both blood clots (pulmonary emboli), fat deposits (fat emboli) or partial collapse of the lungs after general anesthesia. Pulmonary and fat emboli can be life threatening or fatal in some circumstances. Air travel, inactivity and other conditions may increase the incidence of blood clots traveling to the lungs causing a major blood clot that may result in death. It is important to discuss with your physician any past history of blood clots or swollen legs that may contribute to this condition. Cardiac complications are a risk with any surgery and anesthesia, even in patients without symptoms. If you experience shortness of breath, chest pains, or unusual heart beats, seek medical attention immediately. Should any of these complications occur, you may require hospitalization and additional treatment.
Female Patient Information
It is important to inform your plastic surgeon if you use birth control pills, estrogen replacement, or if you believe you may be pregnant. Many medications including antibiotics may neutralize the preventive effect of birth control pills, allowing for conception and pregnancy.
Intimate Relations After Surgery
Surgery involves coagulating of blood vessels and strenuous activity of any kind may open these vessels leading to a bleed, or hematoma. Activity that increases your pulse or heart rate may cause additional bruising, swelling, and the need for return to surgery and control bleeding. It is wise to refrain from strenuous exercise and sexual activity until your physician states it is safe.
Long-Term Results
Subsequent alterations in nasal appearance may occur as the result of aging, weight loss or gain, sun exposure, pregnancy, menopause, or other circumstances not related to nasal surgery. Future surgery or other treatments may be necessary.
Mental Health Disorders and Elective Surgery
It is important that all patients seeking to undergo elective surgery have realistic expectations that focus on improvement rather than perfection. Complications or less than satisfactory results are sometimes unavoidable, may require additional surgery and often are stressful. Please openly discuss with your surgeon, prior to surgery, any history that you may have of significant emotional depression or mental health disorders. Although many individuals may benefit psychologically from the results of elective surgery, effects on mental health cannot be accurately predicted.
Medications
There are many adverse reactions that occur as the result of taking over-the-counter, herbal, and/or prescription medications. Be sure to check with your physician about any drug interactions that may exist with medications which you are already taking. If you have an adverse reaction, stop the drugs immediately and call your plastic surgeon for further instructions. If the reaction is severe, go immediately to the nearest emergency room. When taking the prescribed pain medications after surgery, realize that they can affect your thought process and coordination. Do not drive, do not operate complex equipment, do not make any important decisions, and do not drink any alcohol while taking these medications. Be sure to take your prescribed medication only as directed.
Health Insurance
Most health insurance companies cover surgical operations to treat acute nasal injuries causing nasal obstruction. Coverage for future reconstructive procedures following nasal injuries can vary, depending on your health care insurance company’s policies. Most insurance plans exclude coverage for cosmetic, secondary or revisionary surgery. Please carefully review your health insurance subscriber-information pamphlet.
There are many variable conditions that may influence the long-term result from rhinoplasty and/or septoplasty surgery. Secondary surgery may be necessary to obtain optimal results. The practice of medicine and surgery is not an exact science. Although good results are expected, there is no guarantee or warranty expressed or implied, on the results that may be obtained. In some situations, it may not be possible to achieve optimal results with a single surgical procedure.
Patient Compliance
Follow all physician instructions carefully; this is essential for the success of your outcome. It is important that the surgical incisions are not subjected to excessive force, swelling, abrasion, or motion during the time of healing. Personal and vocational activity needs to be restricted. Protective dressings and splints should not be removed unless instructed by your plastic surgeon. Successful post-operative function depends on both surgery and subsequent care. Physical activity that increases your pulse or heart rate may cause bruising, swelling, fluid accumulation and the need for return to surgery. It is wise to refrain from intimate physical activities after surgery until your physician states it is safe. It is important that you participate in follow-up care, return for aftercare, and promote your recovery after surgery.
Financial Responsibilities
The cost of surgery involves several charges for the services provided. The total includes fees charged by your doctor, the cost of surgical supplies, anesthesia, laboratory tests, and possible outpatient hospital charges, depending on where the surgery is performed. Depending on whether the cost of surgery is covered by an insurance plan, you will be responsible for necessary co-payments, deductibles, and charges not covered. Additional costs may occur should complications develop from the surgery. Secondary surgery or hospital day surgery charges involved with revisionary surgery would also be your responsibility.