Breast Augmentation Risks
Consultations offered at our three convenient locations in Encino, Glendale and Bakersfield
What Are the Potential Risks and Complications of Breast Augmentation with Saline and Silicone Breast Implants?
Contents
- 1 Bleeding
- 2 Infection
- 3 Seroma
- 4 Pain
- 5 Scarring
- 6 Skin Discoloration/ Swelling
- 7 Sutures
- 8 Delayed Healing
- 9 Alteration in Nipple Sensation
- 10 Implant Displacement and Tissue Stretching
- 11 Asymmetry
- 12 Symmastia
- 13 Bottoming Out
- 14 Implant rupture
- 15 Capsular Contracture
- 16 Calcifications
- 17 Silicone Gel Bleed
- 18 Implant Extrusion/ Tissue Necrosis
- 19 Anesthesia
- 20 Damage to Deeper Structures
- 21 Cardiac and Pulmonary Complications
- 22 Breast Disease
- 23 Mammography
- 24 Breast Feeding
- 25 Mondor’s Bands (Cords)
Bleeding
While this is unusual, it is possible to experience a bleeding episode following surgery. If this occurs, emergency treatment to drain accumulated blood, or a blood transfusion, may be required. You can reduce this risk by not taking any aspirin or anti-inflammatory medications for ten days before or after surgery. Non-prescription “herbs” and dietary supplements can also increase the risk of bleeding. The risk of major bleeding, or blood collection, is only about three percent. Most women lose about two test tubes of blood during surgery. Any blood clots that form must be removed in a later surgical procedure.
Infection
Seroma
Sometimes blood in the depth of the breast tissue can accumulate and form a blood collection, called a Hematoma. Seroma is a fluid that arises from the breakdown of accumulated blood or Hematoma. Seroma and Hematoma can accumulate in the breasts, especially following trauma or vigorous exercise. Additional treatment may be necessary to drain the accumulation of fluid around the breast implants.
Pain
All implant patients will experience a degree of pain, as is true of any major surgery. The pain is slightly more pronounced when implants are placed under the muscle. Also, women who have not yet experienced childbirth will probably have a higher degree of pain. Most women report that the pain is greatest in the first 48 hours within surgery. Your cosmetic surgeon will prepare you to address the pain, with a prescription for it prior to your surgery. Prolonged or chronic pain could occur as a result of capsular contraction, nerve entrapment or injury, or even without any specific reason. Removal of implants may not alleviate chronic pain.
Scarring
The location of a scar depends upon which incision technique is used by your cosmetic surgeon. Patients experience scarring differently – some are more delicate than others, and certain ethnic groups are more prone to scarring. Scars will fade with time, but will always be visible to a degree. Most women accept this as the trade-off for having a fuller and prettier breast.
Skin Discoloration/ Swelling
Some bruising and swelling normally occurs after Breast Augmentation. The skin in or near the surgical site can appear either lighter or darker than surrounding skin. Although uncommon, swelling and skin discoloration may persist for long periods of time and, in rare situations, may be permanent.
Sutures
Most surgical techniques use deep sutures. You may notice these sutures after your surgery. Sutures may spontaneously poke through the skin, become visible or produce irritation that requires suture removal.
Delayed Healing
Wound disruption or delayed wound healing is possible. Some areas of the breast skin or nipple region may not heal normally and may take a long time to heal. Areas of skin or nipple tissue may die. This may require frequent dressing changes or further surgery to remove the non-healed tissue. Individuals who have decreased blood supply to breast tissue from past surgery or radiation therapy may be at increased risk for wound healing and poor surgical outcome. Smokers have a greater risk of skin loss and wound healing complications.
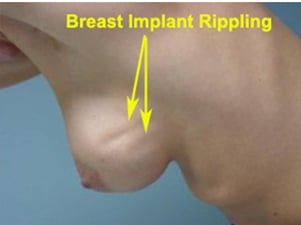
Skin Wrinkling and Rippling
Alteration in Nipple Sensation
After surgery women can experience reduction in nipple or breast sensation as a result of temporary swelling. After swelling subsides there can be an increase or decrease in nipple sensation. FDA studies of 2000 showed loss of nipple sensation in 8-10% of women at three years and 10% at five years. Hypersensitivity of nipple sensation was reported in five to nine % of women at three3 years and 10% at five years.
In my own practice, approximately five percent of patients lose all feelings in one nipple, 10% lose some feeling, and 85% lose no feelings in their nipples. This has been true however the implants have been inserted.
Implant Displacement and Tissue Stretching
Displacement, rotation, or migration of a breast implant may occur from its initial placement and can be accompanied by discomfort and/or distortion in breast shape (visible rippling of the skin). Unusual techniques of implant placement may increase the risk of displacement or migration. Additional surgery may be necessary to attempt to correct this problem. It may not be possible to resolve this problem once it has occurred.
Asymmetry
As is true in nature, no two breasts are identical, even after Breast Augmentation. Some women may require a corrective second surgery if the difference is significant; however, it is usually not any more noticeable than when breasts are a somewhat different size in their natural state.
Symmastia
Symmastia is when both breasts join each other in a single pocket due to the loss of the cleavage fold. This can happen when the diameter of the two implants is greater than that of the chest, or by excessive thinning out of the skin, or by technical errors during surgery. Fortunately, Symmastia occurs very rarely. Unfortunately, its repair is difficult, requiring exchange of implants for smaller ones, and recreation of the cleavage fold with the aid of internal sutures.
Bottoming Out
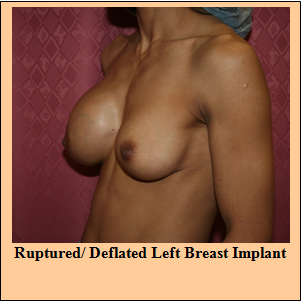
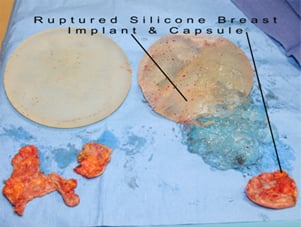
Implant rupture
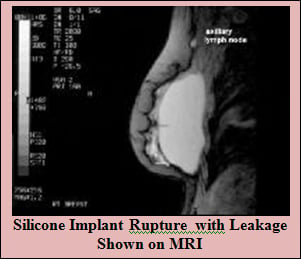
Prospective studies of saline-filled breast implants approved by FDA in May 2000 showed rupture/deflation rates of 3-5% at 3 years and 7-10% at 5 years for augmentation patients. The same studies showed rupture/deflation rates of 6-9% at 3 years and 8-18% at 5 years for reconstruction patients. The newer implants have a less chance of rupture which is about 5-10% at 10 years. As discussed in the earlier section the implants that we use have manufactures warranty against implant rupture.
According to the FDA, placement of the implant through the belly button (TUBA) and closed Capsulotomy damages the implant and increases their rate of rupture.
Several tests are used to evaluate a patient for the rupture of their implant, including Magnetic Resonance Imaging (MRI), mammogram, and ultrasound.
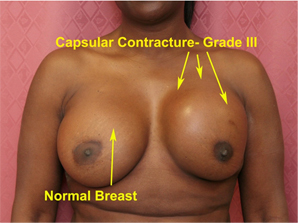
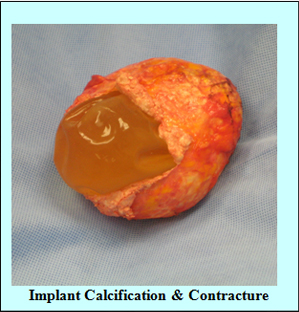
Capsular Contracture
Sometimes, the degree of scarring around the implant is such that the breast begins to feel hard and in extreme cases painful. It may occur in one side, both sides, or not at all. There are four grades of capsular contracture – Baker grades I through IV.
The Baker grading is as follows:
| Grade I | the breast is normally soft and looks natural |
| Grade II | the breast is a little firm but looks normal |
| Grade III | the breast is firm and looks abnormal |
| Grade IV | the breast is hard, painful, and looks abnormal. |
Capsular Contracture may be more common following infection, hematoma, and seroma. However, it is not known for sure why Capsular Contracture happens. The literature also discusses other factors, such as a textured implant surface and submuscular placement of the implant, which may decrease the capsular contracture rate.
Another surgery may be needed to correct Capsular Contracture, usually for grade III or IV. The surgical procedures range from removal of the implant capsule tissue with or without replacement of the implant itself. Capsular contracture may happen again, even after further surgery.
Prospective studies of saline-filled breast implants approved by FDA in May 2000 showed rates of grade III or IV Capsular Contracture of 9% at 3 years and 10-11% at 5 years for augmentation patients. The same studies showed rates of grade III or IV capsular contracture of 25-30% at 3 years and 29-36% at 5 years for reconstruction patients.
Calcifications

Silicone Gel Bleed
Small amounts of silicone gel material seep out through the silicone filled implant shell, and coat the outside of the implant. This material can be felt and seen when a silicone implant is being removed by a surgeon. Scientific studies have shown that this silicone does get into the surrounding lymph nodes and blood stream, but no harm has ever been documented experimentally or clinically.
Implant Extrusion/ Tissue Necrosis
Anesthesia

Damage to Deeper Structures
There is the potential for injury to deeper structures including nerves, blood vessels and muscles and lungs (pneumothorax) during this surgical procedure. The potential for this to occur varies according to the type of procedure being performed. Injury to deeper structures may be temporary or permanent.
Cardiac and Pulmonary Complications
Breast Disease
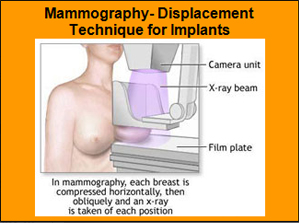
Mammography
Breast implants may make mammography more difficult and may obscure the detection of breast cancer. Any breast implant can impair the detection of breast cancer, regardless of the type of implant or where it is placed in relation to the breast. Implant rupture can occur from breast compression during mammography. Inform your mammography technologist of the presence of breast implants so that appropriate mammogram studies may be obtained. Patients with Capsular Contracture may find mammogram techniques painful and the difficulty of breast imaging will increase with the extent of contracture. Ultrasound, specialized mammography and MRI studies may be of benefit to evaluate breast lumps and the condition of the implant(s). Because more x-ray views are necessary with specialized mammography techniques, women with breast implants will receive more radiation than women without implants who receive a normal exam. However, the benefit of the mammogram in finding cancer outweighs the risk of additional x-rays. Patients may wish to undergo a preoperative mammogram and another one after implantation to establish a baseline view of their breast tissue. You may be advised to undergo a MRI study in the future to verify the condition of your breast implants inside your body.
Breast Feeding
Breast milk is the best food for babies. Many women with breast implants have successfully breast fed their babies. It is not known if there are increased risks in nursing for a woman with breast implants. A study measuring elemental silicon (a component of silicone) in human breast milk did not indicate higher levels from women with silicone-filled gel implants when compared to women without implants. Cow’s milk contains higher levels of elemental silicon as compared to human milk. Implant placement techniques that involve incisions through the nipple and areola locations may reduce the ability to successfully breast feed. If a woman has undergone a mastectomy, it is unlikely that she would be able to breast feed a baby on the side where the breast was removed.
Mondor’s Bands (Cords)
This condition, named after French surgeon Henri Mondor, occurs when the vein appearing to be a tender cord that runs vertically below the inframammary fold becomes inflamed. This usually corrects itself after a few weeks, and following treatment with warm, moist compresses.
Immune System Diseases
A small number of women with breast implants have reported symptoms similar to those of known diseases of the immune system, such as systemic lupus erythematosus, rheumatoid arthritis, scleroderma, and other arthritis-like conditions. To date, after several large epidemiological studies of women with and without implants, there is no scientific evidence that women with either saline-filled or silicone gel-filled breast implants have an increased risk of these diseases. These diseases appear no more common in women with implants than those women without implants. The effect of breast implants in individuals with pre-existing immune system and connective-tissue disorders is unknown. There is the possibility of unknown risks associated with silicone breast implants and tissue expanders.
Summary of Saline Breast Augmentation Complication Rate:
(Source: 2004/ A95 Inamed Study, n=901)
| Complications | N = 901 Patients | |
3-Year** Complication Rate | 5-Year Complication Rate | |
| Additional Operation (Re-operation) | 21% | 26% |
| Breast Pain* | 16% | 17% |
| Wrinkling* | 11% | 14% |
| Asymmetry* | 10% | 12% |
| Implant Palpability/Visibility* | 9% | 12% |
| Implant Replacement/Removal for Any Reason | 8% | 12% |
| Capsular Contracture | 9% | 11% |
| Intense Nipple Sensation* | 9% | 10% |
| Loss of Nipple Sensation* | 8% | 10% |
| Implant Malposition* | 8% | 9% |
| Intense Skin Sensation* | 7% | 8% |
| Scarring Complications | 6% | 7% |
| Leakage/Deflation | 5% | 7% |
| Irritation/Inflammation* | 3% | 3% |
| Seroma | 3% | 3% |
| Hematoma | 2% | 2% |
| Skin Rash | 2% | 2% |
| Capsule Calcification* | 1% | 2% |
| Delayed Wound Healing* | 1% | 1% |
| Infection | <1% | 1% |
Note: *These complications were assessed with severity ratings. Only the rates for moderate, severe, or very severe (excludes mild and very mild ratings) are shown in this table.
** As reported in original PMA submission.
Dr. S. Sean Younai, MD, FACS